NEWBORN HEAD SHAPE: WHAT IS NORMAL?
Following the birthing process, it is very common for a newborn’s head to be elongated or have an odd shape. Although babies may have an uneven head shape at birth however this should remould to a normal more symmetrical shape within 6 weeks after birth. Flattening of your baby’s head can occur when constant pressure is applied to one part of a baby’s head.
When babies are born, the bones of their skull are thin and flexible, meaning the head is soft and may change shape easily. All babies should have two soft areas at the top of their head (fontanelles). These fontanelles allow for your baby’s rapidly growing brain during infancy and usually close around the age of 12 months.

https://generalhappenings.files.wordpress.com/2012/01/mchnewbornexam2.jpg
Plagiocephaly describes a condition where your baby’s head is not symmetrical. If your baby has plagiocephaly, it is important to determine if the fontanelles have closed too early. This is a condition called craniosynostosis. It is estimated to occur in 1 / 2500 live births and should be reviewed by a doctor.
Positional plagiocephaly describes a condition where your baby’s head is not symmetrical but the fontanelle remain open. Positional plagiocephaly does not affect the development of your baby’s brain however, it may alter your baby’s physical appearance as it can cause uneven growth of their head or face. Positional plagiocephaly is a relatively common condition occurring in an estimated 10-50% of newborns. In infants 7-12 weeks of age, it occurs in about 46% of babies.
.jpg)
Normal head shape (left image)
Back of head is round on both sides Ear position is level
Ear position is level Both sides of the forehead look symmetrical
Positional plagiocephaly (right image)
Flattened area on the back of the skull or either side of the head
One ear may be more forward than the other
One side of the forehead may protrude more than the other side
Studies have found babies to be more likely to have positional plagiocephaly if they have the following characteristics:
• First born
• Premature
• Male
• Difficult or assisted birth
• Breech positioning during the last trimester
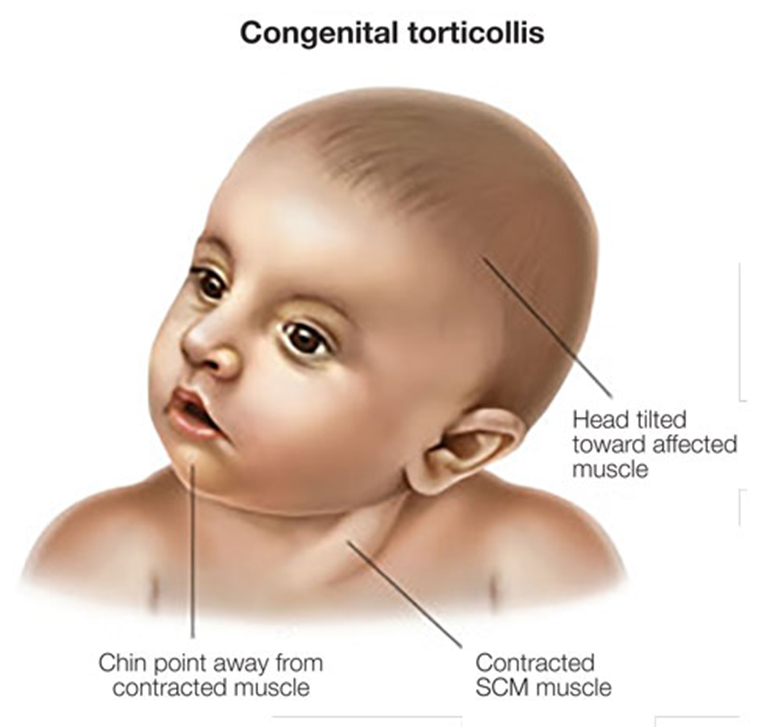
• Other neck problems e.g. congenital muscular torticollis
• Lack of supervised tummy time when awake i.e. less than 3 times per day
• Always positioned to the same side when feeding or sleeping
Positional plagiocephaly: What can you do?
For the majority of children, positional plagiocephaly is a correctable condition.
For most babies, regular repositioning of your baby’s head before they are 4 months old will result in optimal outcomes. If your baby has a flat spot, alternating their head position can improve this.
Positional plagiocephaly can also be associated with asymmetrical neck muscles also know as torticollis. Some babies have neither of these condition, some may have one of these conditions and other babies may have both positional plagiocephaly and torticollis. Treatment of torticollis and positional plagiocephaly will have similar aspects. Both of these conditions can be improved with physiotherapy assessment, treatment and a home program of positioning and play.
Key points to remember
• Babies may have an uneven head shape at birth however this should remould to a normal more symmetrical shape within 6 weeks after birth.
• Positional plagiocephaly will not affect the development of your baby’s brain.
• If you are concerned about your baby’s head shape, talk to your Child Health Nurse, GP, paediatrician or paediatric physiotherapist.
• A paediatric physiotherapist can assess your child and assist with planning a home program which may include specific exercises, stretches and promotion of a variety of positions during awake, sleep and play time.
If you would like to book an appointment for your child with Tanya at Bathurst Family Physiotherapy please call one of our friendly reception staff on (02) 6331 8354
REFERENCES:
https://www.physiotherapy.asn.au/APAWCM/Physio_and_You/Infants.aspx
https://www.rch.org.au/uploadedFiles/Main/Content/plastic/Deformational_Plagiocephaly.pdf
http://www.rch.org.au/kidsinfo/fact_sheets/Plagiocephaly_misshapen_head/
https://www.schn.health.nsw.gov.au/parents-and-carers/our-services/craniofacial/chw
http://www.mayoclinic.org/diseases-conditions/craniosynostosis/symptoms-causes/dxc-20256926



.jpg)
